Navigating the world of therapy can be daunting, especially when faced with an array of acronyms and complex terminologies. Two of the most effective and well-known therapeutic approaches are Cognitive Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT). Both are recognized as powerful tools for managing various mental health disorders, but their application and focus can differ significantly.
At Madison Park Psychological Services, we’re here to shed light on the fundamental aspects of both DBT and CBT, empowering you to make informed decisions about your mental health.
Dialectical Behavior Therapy vs. Cognitive Behavioral Therapy: What’s the Difference?
CBT vs. DBT: Understanding the Similarities and Differences
Understanding the Differences Between CBT vs DBT
Together we’ll explore the intricacies of DBT vs CBT, including how each approach is similar and unique, and discover how each can be an empowering tool to help you overcome various mental health challenges. This exploration aims to equip you with a clear understanding and guide you in choosing the most suitable therapy for your unique needs.
DBT and CBT, both well-established and evidence-based therapies, provide unique frameworks for understanding and addressing mental health disorders. Rooted in cognitive psychology, they utilize talk therapy to address negative thought patterns leading to destructive behaviors.
CBT, often referred to as the “gold standard” of psychotherapy, concentrates on the present. It operates on the principle that our thoughts, feelings, and behaviors are all interconnected and influential of one another. A main principle of CBT is that if you can recognize negative thinking and behavioral patterns, you can then alter them for more adaptive ones that improve your mood and life overall. CBT is used in treating many mental health conditions, including anxiety, panic disorder, phobias, OCD, trauma, and depression.
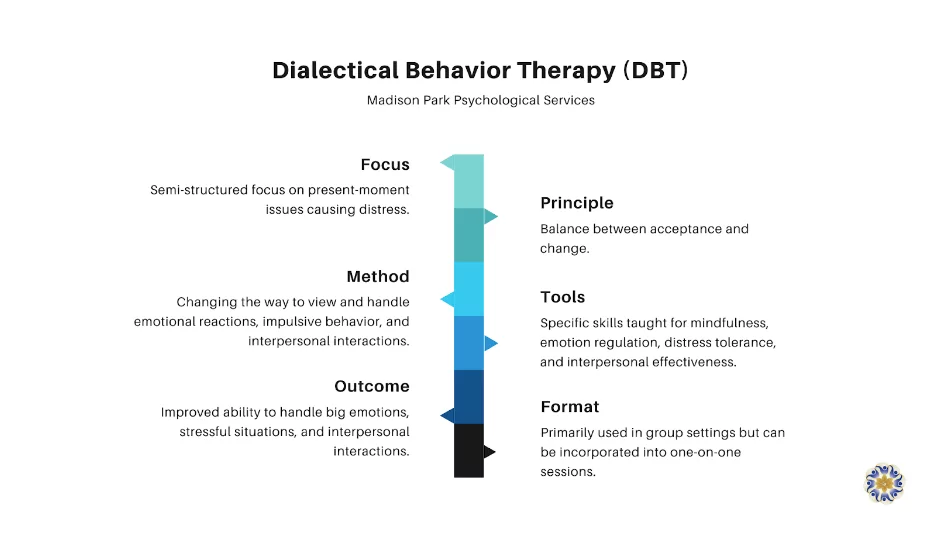
DBT was initially created for those with Borderline Personality Disorder (BPD) but has since been indicated for a range of other conditions. While CBT primarily focuses on change, DBT focuses on giving equal weight to acceptance and change (hence, “dialectical”) so that you can both accept where you are right now and strive for better at the same time. This modality places great emphasis on regulating your emotions, improving your ability to handle distress, and having effective interpersonal interactions.
While DBT is influenced by CBT, it takes a more holistic approach. DBT focuses on changing destructive behaviors, and gives credence to mindfulness. It incorporates concepts such as acceptance and validation into its framework, yet also challenges you to make gradual shifts so that, ultimately, you can lead a better life.
DBT was initially designed to treat individuals with BPD, particularly those struggling with extreme behaviors, including suicidality. It is primarily used in a group setting, which allows participants to gain support from peers who are facing similar struggles. In more intensive DBT-specific programs, a typical DBT therapy protocol may involve group and individual sessions, specific skills training, and regular phone coaching multiple times per week. At an outpatient private practice, like ours, typically you can receive DBT in a weekly small group format and/or individual sessions. The emphasis is placed on teaching skills in four key areas: mindfulness, interpersonal effectiveness, emotional regulation, and distress tolerance.
DBT’s focus on acceptance comes from dialectical philosophy, which stresses the balance and integration of opposites. In the context of therapy, this means accepting yourself as you are, while also working towards change. This acceptance is crucial for those struggling with feelings of worthlessness or self-hatred, as it fosters a non-judgmental environment where they can begin to work through issues.
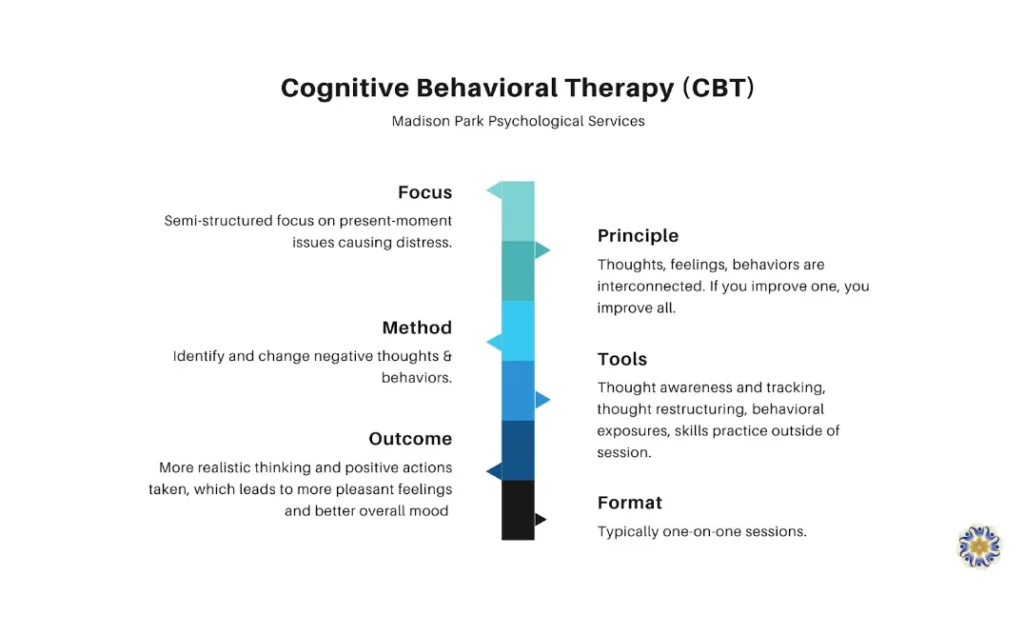
CBT is a form of talk therapy designed to help you manage your mental health difficulties by changing the way you think and behave. It is commonly used to treat a wide range of issues, including anxiety, panic, OCD, phobias, trauma, depression, among others.
The key principle behind CBT is that our thoughts, feelings, and behaviors are all interconnected and influential of one another. This means that by modifying our negative thoughts and dysfunctional beliefs, we can change the way we feel and behave. CBT focuses on the here and now, often disregarding the past in favor of tackling current issues that cause distress. It helps you slow down and become mindful of your thought process and behaviors to identify maladaptive patterns that can be altered. Your CBT therapist will provide concrete tools meant to challenge and replace negatively biased thoughts and beliefs with more realistic ones. In some cases, you might also be guided to undertake new behavioral actions, also known as “exposures,” helping you practice acting in new, more beneficial ways. This process centers around gradually confronting and managing feared or avoided situations, thoughts, or feelings. Exposures can be a powerful tool in the treatment of anxiety-related disorders, phobias, and OCD. Through exposures, you learn to reduce the fear or distress associated with specific triggers, ultimately leading to improved coping mechanisms and increased confidence in managing challenging situations.
CBT is typically administered in one-on-one therapy sessions, which tend towards semi-structured and goal-oriented. You and the therapist work together to identify and understand your negative thought patterns, first by becoming aware of, and tracking, them. Once these have been identified, your therapist guides you to challenge and restructure these thoughts and beliefs by replacing them with more realistic alternatives.
When in CBT treatment, not only do you work on your thoughts and behaviors within the session, but also outside of it. Out-of-session tasks are designed to reinforce the skills learned during therapy sessions and encourage you to practice these new strategies in your daily life.
CBT also places emphasis on learning. The aim is to equip you with the skills you need to ultimately be your own therapist, allowing you to continue to improve your mental health long after their therapy sessions have ended.
DBT and CBT share a common goal: to help individuals manage their mental health issues by changing their patterns. While they each have their unique methods and areas of focus, integrating these two therapeutic approaches can often yield beneficial results.
The integration of DBT and CBT creates a comprehensive treatment plan that addresses a wide array of mental health disorders. While CBT focuses on identifying and changing negative thought and behavior patterns, DBT emphasizes both acceptance and change and teaches you how to manage big emotions, stressful situations, and relationships. By drawing from both these therapies, mental health professionals can tailor a more nuanced treatment approach to match your unique needs and circumstances.
For example, consider an individual dealing with intense emotional responses. They may benefit from DBT’s emphasis on emotional regulation and distress tolerance, but they might also benefit from CBT’s focus on changing negative thought patterns that may contribute to these emotional responses. By integrating both DBT and CBT, the therapist can help the patient manage their emotions and alter their thinking patterns simultaneously.
The addition of DBT’s group therapy component can complement CBT’s individualized sessions. Group therapy provides an opportunity for folks to share their experiences, gain support, and learn from others dealing with similar issues, which can be a valuable supplement to one-on-one therapy.
Present-moment awareness, or the practice of slowing down to determine exactly what’s going on for you in the moment, plays a role in both DBT and CBT. It is a tool used to help individuals observe their thoughts, feelings, and/or behaviors from a non-judgmental place. Despite being a component of both therapies, awareness is used differently within each.
In DBT, awareness takes on the form of mindfulness, which is a foundational skill that supports all other strategies. It is considered a critical element for achieving balance and acceptance. Mindfulness practices in DBT might involve exercises that enhance awareness of one’s bodily sensations, thoughts, and environment, promoting non-judgmental acceptance of the present moment.
In contrast, CBT uses awareness as a tool to support the process of cognitive restructuring, or changing your thought and belief patterns. By increasing awareness of thoughts and feelings, awareness enables you to recognize negative thought patterns and actions as they occur. This awareness can be pivotal in challenging these patterns and replacing them with better alternatives.
At Madison Park Psychological Services, our team of therapists is skilled in both DBT and CBT modalities. We believe in personalized treatment plans tailored to each individual’s unique needs and circumstances. Whether it’s CBT, DBT, or a combination of both, our therapists will work with you to determine what best suits your needs.
Reach out to us today to schedule a session with one of our therapists and begin your journey toward improved mental health.
To contact us or book an appointment, please complete the form below.